In 10 seconds? Some experts argue that it’s not worth screening for prostate cancer. While the procedure has decreased prostate cancer mortality, it has also led to high numbers of harmless cancers being flagged, which leads to more harm than good.
Sorry but that sounds like abandoning people with positive cases... OK, I know it might sound controversial at first but consider this: most prostate cancers aren’t destined to spread. It’s been discovered that the majority of diagnosed prostate cancers (55%) are unlikely to ever cause symptoms or negatively impact patient survival. This finding is supported by autopsy data showing that many men over the age of 60, who died of other causes, had evidence of prostate cancer. In other words, many men die with prostate cancer, but not of prostate cancer.
But surely it’s better to be safe than sorry with cancer? It turns out that ‘safety’ is not so straightforward with cancer. A cancer diagnosis (AKA a doctor telling you that you have cancer) by itself is far from benign. Patients who receive treatments for prostate cancer commonly develop long-lasting side effects (like impotence and bowel problems). To that point, it’s been estimated that more than 1 million men have been treated for prostate tumors that likely would have never caused symptoms. Of course, beyond side effects, cancer treatment comes with a considerable amount of stress for the patient (“OMG, I’ve got cancer!”) and a hefty price tag.
OK, but we still need to detect 'bad cases'… how do they screen for prostate cancer? A blood test that can detect prostate cancer, called the Prostate Specific Antigen, or PSA test, has been implemented in healthcare settings since the late 1980s. The PSA test has made it so that prostate cancer is diagnosed much more frequently.
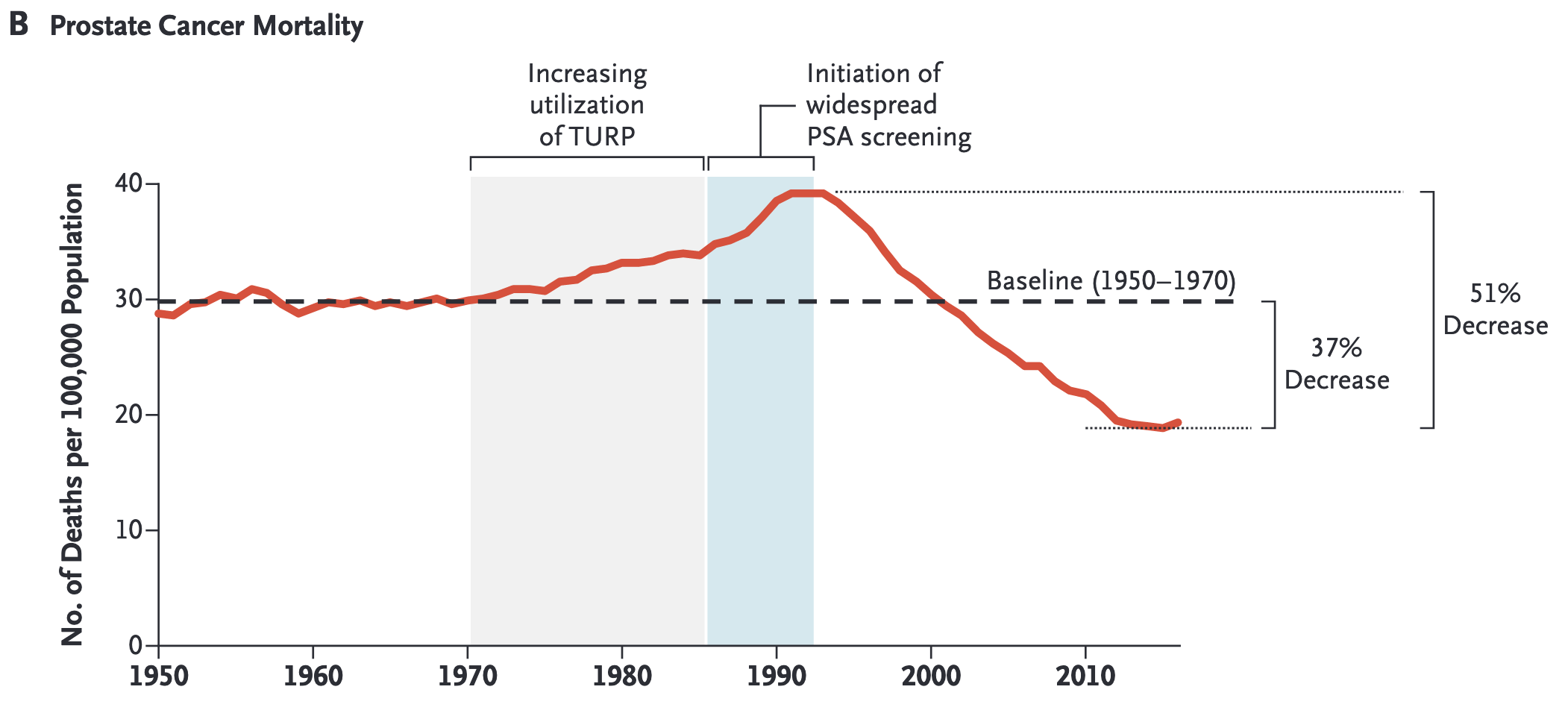
So, what’s the problem with it? Well, there is good news and there is a problem. The good news is that, since the implementation of PSA testing, prostate cancer mortality has dropped by about 37%. This showcases the merit of the PSA test in detecting cancer before it spreads (a major goal of cancer screening) and the success of effective cancer treatments (largely hormonal adjuvant therapy) for these early-stage tumors. However, it also leads to the diagnosis of cancers which would otherwise just tick along and cause no harm. But treating these cancers does cause harm.
So, what’s the solution? Ideally, prostate cancer screening needs to be improved so that people are only diagnosed (again, told they have prostate cancer) if the tumors are likely to be problematic. Because of all the controversy, the US Preventive Services Task Force, a major influencer in national cancer testing guidelines, removed PSA testing from its recommendations. Some doctors still choose to prescribe PSA testing but are urged to carefully communicate the nuances of a positive result with patients.
Trading one cause of death for another
Many cases of prostate cancer occur in men over 70. But it’s important to keep in mind that men in the USA only have an average life expectancy of 74.5 years old.
Experts point out that just because PSA testing may decrease prostate cancer mortality doesn’t mean that overall life is extended or quality of life is increased.
This point has been showcased in colorectal cancer screening. This study shows that although patients screened and treated for colon cancer are less likely to die of colon cancer, that doesn’t mean that they are destined to live longer overall–essentially swapping out one cause of death for another. All these findings add nuance to discussions on best practices for cancer prevention.
Dr. Talia Henkle has distilled 4 papers saving you 14 hours of reading time.

The Science Integrity Check of this 3-min Science Digest was performed by Flávia Oliveira Geraldes






